All this makes effective communication with the patient our main goal, to save time for both the patient and the staff. If everyone understands the messages they hear in the same way we can avoid mistakes and misinterpretations. This way the patient can really feel taken care of – especially if they are already having a hard time due to the medical condition which brought them to the facility in the first place. How to achieve that?
What is communication?
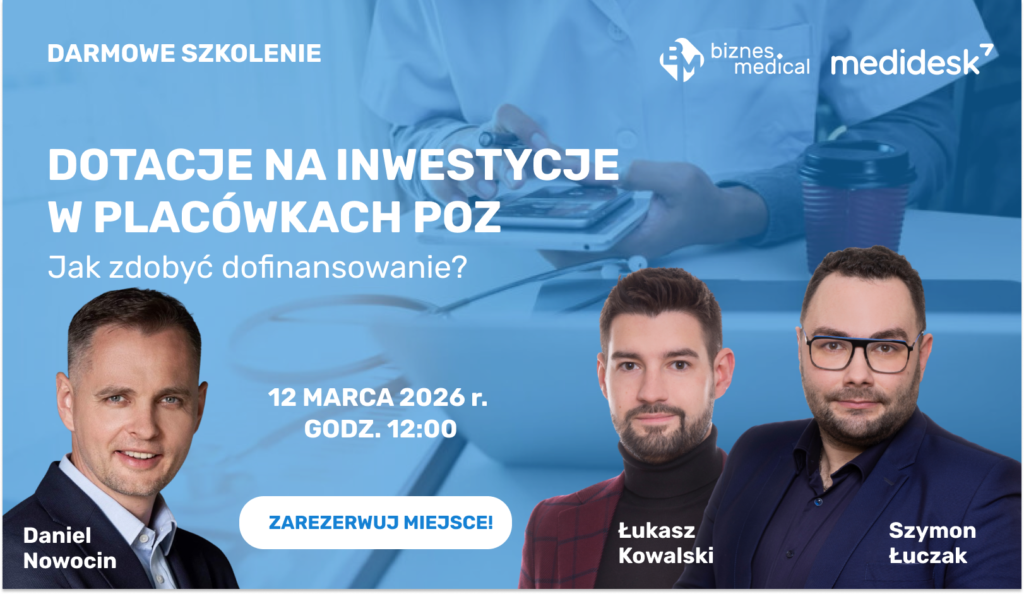
The word communication derives from the Latin verb communico, communicare. It means sharing a message with someone, consulting, making something common. Nowadays by the term communication, we understand the process of communication between individuals, institutions, or groups. Each time the purpose of this activity is to exchange thoughts, share information or knowledge. In our case, we are particularly interested in interpersonal communication, i.e. communication between two persons: a patient and an employee of a medical institution. It is usually characterized by the direct presence of both interlocutors, so it is called face-to-face communication. For both to run smoothly, it is important that the registrar has the right qualifications and learned behaviors. Principles of proper communication with the patient can be learned at professional training courses, organized by Medidesk specialists. Our trainers have years of experience working with medical entities, so the knowledge they pass on helps improve not only verbal but also non-verbal communication among staff.
What is verbal and non-verbal communication?
Verbal communication is the primary mode of human communication by using speech. Every time we engage in a dialogue with someone, we participate in verbal communication. What is important, however, is that it is constantly accompanied by non-verbal communication. It consists of our behavior, gestures, facial expressions. We can also convey information to our interlocutor with a shrug of the shoulders, a glance, or a facial expression – sometimes unconsciously, against our will.
Effective communication with a patient requires not only a properly conducted conversation but also communicating the same information by non-verbal means. In such a situation they should understand us and give us the expected answer. Often, however, this does not happen for a simple reason – there are communication barriers between the patient and the health care provider that make understanding difficult.
What are communication barriers?
The terms communication barriers or blockages in our case refer to external actions or factors through which effective communication with the patient is hindered. Thomas Gordon – an American psychologist, psychotherapist, and family counselor – formulated a list of twelve barriers to communication in his books „Raising Without Failure” and „How to Live Well with People” formulated a list of twelve blocks to interpersonal communication. This is a list of the most common mistakes that make it difficult to get along with others, commonly known as „Gordon’s 12 barriers” or „the dirty twelve destroyers of communication”. Of the barriers included on this list, the most significant from the point of view of the healthcare provider include criticizing, ordering, or moralizing – often these can take the form of sentences such as „it’s your fault you’re overweight”, „you have to provide prior medical records today, I don’t care how”, or „you shouldn’t smoke in your condition”. When talking to a patient, both the registration clerk and the nurse or doctor should avoid these comments. Otherwise, they will put negative pressure on the patient or make him feel guilty, which certainly does not promote mutual cooperation.
The types of barriers which occur in communication between humans
A much more interesting classification was compiled by Prof. Gabriel Łasiński in the year 2000. In his book entitled “The art of presentation,” he indicated several barriers, dividing them into three major categories:
- semantic barriers
- psychological barriers
- physical or environmental barriers
The most common ones in terms of contacts with patients include using unclear language – when the patient doesn’t know exactly what the front-desk employee or a doctor is saying or understands the terminology which is used differently than it is intended. Another barrier which we observe at medical facilities is the noise during conversations with the registration employee – caused, for example, by a telephone which rings next to the desk or simultaneous conversations of other registration employees with other patients. Among psychological barriers we should focus our attention on negative attitude, shyness, neglecting other people, lack of ability to listen, or simple tiredness. Each of these features may occur in any one conversation and they should all be avoided.
How to deal with those barriers?
As you can see above, communication with a patient may be disrupted by many barriers, which does not necessarily depend fully on us. In case we have no influence on the occurrence of some of those barriers, we may prepare for them to occur. When they do, it will be easier to overcome them.
The basic rule, which effective communication with the patient depends on, is overcoming stress. The patient has the right to be nervous and stressed, but if the medical staff is a walking oasis of peace it should affect the interlocutor. It is equally important to listen actively, which isn’t only about nodding your head – the patient should be asked about details if they were understood correctly. It is also important to ask the right questions to enable a proper response, which will help us avoid miscommunication.
A medical employee doesn’t have to know everything
The most important thing is that a medical employee should know all services and procedures at the given medical facility, which will limit the amount of stress which they experience in conversations when patients ask questions. Nevertheless, don’t be afraid of your lack of knowledge: nothing bad will happen if a patient finds out from a staff member that they aren’t able to provide complete information. It is much more valuable for both sides when the employee admits that they have to verify something and get back to the patient as soon as possible, than when someone tries to pretend they have all the knowledge and keeps guessing. It is also crucial to properly prepare the M.D. for a consult – they should become familiar with the patient’s medical documentation and history of their condition. The preparation will make the online visit more effective and help avoid any miscommunication.
How else can we facilitate communication with the patient?
The quality of communication between patients and registration staff can be improved by sending employees to professional training courses for medical registrars. They allow you to improve patient service procedures and effectively use available tools that support the process of selling medical services. This increases the effectiveness of employees’ actions, and thus builds better relationships with patients.
Regardless of what the conversation between the patient and the employee is about or how it is going, the most important thing is to have a positive attitude. An upbeat voice from a healthcare professional can have a soothing and calming effect on a nervous and stressed caller, making it easier to connect with the patient. A calm and patient person is not only able to control the conversation by asking the right questions, but also to have a positive influence on the caller – and then effective communication with the patient is within our reach.